Fibromyalgia
Fibromyalgia
Fibromyalgia is a neurosensory disorder marked by persistent musculoskeletal pain and tightness, usually at sore points in the neck, shoulders, chest, back, knees and hips.
The exact cause and underlying mechanisms of fibromyalgia remain unclear. It is thought to be hypersensitivity of the central nervous system, causing muscles and soft tissues to go into spasm (hence the tightness and stiffness of muscles and joints). Patients with fibromyalgia often complain of fatigue, cognitive difficulties, and migraines and various other physical complaints. Disturbed sleep and sometimes depression are often associated with this condition.
Symptoms Of Fibromyalgia
Fibromyalgia causes chronic muscle pain and fatigue. The pain typically originates in one area, usually the neck and shoulders, and then radiates out. Most patients report feeling some pain all the time; and many describe it as “exhausting”. They mimicked arthritis type of pain occurring near shoulders, elbow, hips and knees. Fibromyalgia (also called fibrositis or fibromyositis) is a syndrome that causes chronic, sometimes debilitating, muscle pain and fatigue. The pain occurs in areas where the muscles attach to bone or ligaments, and is similar to the pain of arthritis. The joints themselves are not affected, however, so they are not deformed nor do they deteriorate, as they may in arthritic conditions.
The pain can vary, depending on the time of day, weather changes, physical activity, and the presence of stressful situations; it has been described as stiffness, burning, radiating and aching. The pain is often more intense after disturbed sleep. The other major complaint is fatigue, which some patients report as being more debilitating than the pain. Fatigue and sleep disturbances are, in fact, almost universal in patients with fibromyalgia, and if these symptoms are not present, then some experts believe that physicians should seek a diagnosis other than fibromyalgia. Between a quarter and a third of patients experience depression, and disturbances in mood and concentration are very common. (Up to 46% of patients had been diagnosed with depression in the past.) Fibromyalgia patients are also prone to tension or migraine headaches. Other symptoms include dizziness, tingling or numbness in the hands and feet, and gastrointestinal problems, including irritable bowel syndrome with gas and alternating diarrhoea and constipation. Some patients complain of urinary frequency caused by bladder spasms. Women may have painful menstrual periods.

Causes of Fibromyalgia
Fibromyalgia is sometimes categorized as primary or secondary; primary fibromyalgia is the more common form.
Primary Fibromyalgia
A dysfunctional disorder caused by a constellation of biologic responses to stress in individuals who are more susceptible to such stress because of negative personal histories or genetic factors. The cause or causes of primary fibromyalgia are not known; this condition is also sometimes referred to as idiopathic fibromyalgia. Many experts believe that fibromyalgia is not a disease but, rather, a dysfunctional disorder caused by a constellation of biologic responses to stress in individuals who are more susceptible to such stress because of negative personal histories or genetic factors.
Family Factors
Chronic Sleep Disturbance
Abnormalities in the Brain
Auto-immunity
Post-Traumatic Stress Disorder
Hypervigilance
Muscle Cell Abnormalities
Secondary Fibromyalgia
Secondary fibromyalgia is caused by specific disorders, including injury, auto-immune disorder, or surgery. The symptoms are identical to those of primary fibromyalgia but are harder to treat. In one study, secondary fibromyalgia developed in over 20% of patients who had neck injuries.
Diagnosing Fibromyalgia
In spite of increasing evidence that fibromyalgia is a physical disorder, there is no objective method for diagnosing the problem. According to the American College of Rheumatology’s Classification criteria for a diagnosis of fibromyalgia, it requires the presence of at least 11 of 18 specific areas on the body that are intensely painful (not just tender) when pressed.
These trigger points can be found in the following areas (refer to body picture):
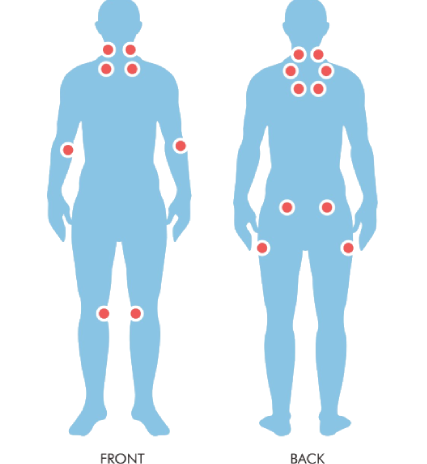
- on left or right side of the back of the neck, directly below the hairline;
- on left or right side of the front of the neck, above the collar bone (clavicle);
- on left or right side of the chest, right below the collar bone;
- on left or right side of the upper back, near where the neck and shoulder join;
- on left or right side of the spine in the upper back between the shoulder blades (scapula);
- on the inside of either arm, where it bends at the elbow;
- on left or right side of the lower back, right below the waist;
- on either side of the buttocks right under the hip bones;
- on either knee cap.
To confirm the diagnosis, widespread pain – which is experienced in upper and lower and left and right parts of the body and in the spine – must persist for at least three months. Using such criteria is helpful in making a diagnosis of fibromyalgia, but it is not completely reliable and misses about 10% of patients. Because the sensitivity of tender points may vary depending on circumstances, a physician may re-check pressure points that do not respond the first time in patients who have other significant symptoms. Some experts believe that fibromyalgia can be diagnosed if only 8 to 10 tender points are identified but the patient also has at least three other relevant symptoms, including morning stiffness, fatigue, sleep disturbance, numbness or tingling in the hands and feet, or headache.
Although symptoms are similar in children, some experts suggest that they often have no set number of pain trigger points. In one study, children had an average of 9.7 trigger point locations, compared to the minimum of 11 in adults. In general, children with fibromyalgia most often experienced sleep disorders and diffused pain, and less frequently headache, general fatigue and morning stiffness.
Medical and Personal History
A physician should always take a careful personal and family medical history, which would include a psychological profile and a history of any factors that might be indicative of disorders other than fibromyalgia, including recent weight change, physical injuries, infectious diseases, muscle weakness, rashes, and any instances of sexual, physical, substance or alcohol abuse. The patient should report any drugs taken, including vitamins and over-the-counter or herbal medications.
Physical Examination
Any physical examination for fibromyalgia requires that the physician press firmly on all potential trigger spots. It also includes scrutiny of nails, skin, mucous membranes, joints, spine, muscles and bones to help rule out arthritis, thyroid disease and other disorders.
Other Tests
In most cases of fibromyalgia, laboratory tests tend to be normal; if they are abnormal, then other disorders should be suspected. Tests for specific diseases may be given if a family history or symptoms of other disorders are present. Sometimes, blood tests, such as thyroid and liver function tests, blood count, tests of certain antibodies, and sedimentation rate, are recommended. Follow-up psychological profile testing may be suggested if laboratory results do not indicate a specific disease. One study found high levels of an auto-antibody called antipolymer antibody in nearly half of fibromyalgia patients, but not in patients with auto-immune diseases, such as rheumatoid arthritis. A test for this antibody is in development, and may help differentiate between fibromyalgia and these other, sometimes similar, disorders.
Risk Factors
Fibromyalgia is the most common cause of widespread muscular pain and affects an estimated 2% of the general population. Two thirds of patients are women, and their symptoms are more severe than mens. An increased incidence of fibromyalgia has been reported in people who have relatives with the disorder, indicating that a genetic component may cause certain people to be more susceptible to fibromyalgia. The disorder usually occurs in people between 20 to 60 years of age and peaks at age 35. In one study, however, fibromyalgia increased with age, and had a prevalence of over 7% in patients between 60 and 79 years of age. A condition called juvenile primary fibromyalgia, which appears in children, is uncommon, but studies indicate that its incidence is increasing. One study found that 1.2% of school children; all girls. met the criteria for fibromyalgia. It can occur in anyone and is more prevalent in females than males. Other studies have found an even higher prevalence of fibromyalgia in children.
Frequently Asked Questions
What Other Conditions Show the Same Symptoms as Fibromyalgia?
Between 10% and 30% of doctors’ visits are due to symptoms that resemble those of fibromyalgia, including fatigue, malaise and general muscle pain. No laboratory test can confirm a diagnosis of fibromyalgia, and if tests for tender spots are ambiguous, physicians will rule out other conditions, including various physical diseases, chronic fatigue syndrome, sleep disturbances, medications, toxins and psychological causes. It should be noted that a diagnosis of any of these disorders may not always rule out fibromyalgia, which can accompany other common and similar conditions.
Chronic Fatigue Syndrome
The two disorders share most of the same symptoms; some patients with CFS even exhibit similar tender pressure points, although muscle pain is less prominent in patients with CFS. The two disorders are even treated almost identically. Fatigue is the dominant symptom in CFS whereas pain with tender points is predominant in fibromyalgia. Some physicians believe that fibromyalgia and CFS are the same and define fibromyalgia as an extreme variant of chronic fatigue syndrome. One physician described the relationship between fibromyalgia and chronic fatigue as similar to one between a migraine and a headache. There is some physical evidence, however, that the two disorders may be distinct, which offers the possibility for treatments that are specific to each. Some research indicates, for example, that patients with fibromyalgia may have high levels of a compound called substance P in their spinal fluid, while CFS patients may not. Levels of substance P change in response to pain.
Myofacial Pain Syndrome
Rheumatoid Arthritis and Other Auto-immune Diseases
Another auto-immune disease is Hashimoto’s thyroiditis, a form of hypothyroidism (low levels of thyroid hormone), which, if undetected, can cause widespread muscle aches, depression and fatigue. Other auto-immune disorders with similar symptoms and with a higher prevalence in women than men are systemic lupus erythematosus (SLE) and multiple sclerosis. Fibromyalgia symptoms, in fact, are very common in SLE patients, although the two conditions are thought to be distinct. Auto-immune diseases evolve slowly, and even when physicians diagnose fibromyalgia, they should keep track of any changes in symptoms over time in order to rule out these other illnesses, which require different treatments.
Other Medical Conditions
Major Depression Disorder
Criteria have been established to help physicians differentiate between normal discouragement experienced by everyone, including fibromyalgia patients, and major depression disorder. Unlike ordinary periods of sadness, an episode of depression usually lasts many months.
Symptoms of depression include:
1. Depressed mood every day
2. Significant weight gain or loss (more than 10% of an individual’s normal body weight)
3. Insomnia or excessive sleeping
4. Restlessness or a sense of being slowed down
5. Low daily energy
6. Worthless or inappropriate guilty feelings
7. An inability to concentrate or to make decisions and
8. Suicidal thoughts. The presence of several of these symptoms suggests depression, rather than fibromyalgia, particularly if the tender points typical of fibromyalgia are not also present.
Sleep Disturbances
Drugs and Alcohol
Chemicals and Other Toxins
How serious is Fibromyalgia?
Fibromyalgia can be mild or disabling, and the emotional repercussions can be substantial. There are estimates that 30% to 40% of patients have had to stop work or change jobs. About half of all patients have difficulty with or are unable to perform routine daily activities. There is some indication that such patients are at higher risk of carpal tunnel syndrome and osteoporosis. The pain, emotional repercussions or sleep disturbances may lead to self-medication and overuse of sleeping pills, alcohol, drugs or caffeine.
Desperation may encourage a belief in false cures and potentially dangerous use of herbal or so-called natural remedies. Although the disease is chronic, it is neither progressive nor fatal, and remission can occur in many patients who participate in disease management programs. Children with fibromyalgia tend to have a better outlook than adults. In adult patients who were studied for four and a half years, those who had adequate exercise had the most promising outcome; those with a significant life crisis or who were on disability had a poorer outcome than others. Outcome was determined by improvements in the patients’ capacity to work, their own feelings about their condition, pain sensation, disturbed sleep, fatigue and depression..
Treatment Options
Experts recommend a multi-faceted approach to treating fibromyalgia that involves exercise to reduce pain and strengthen muscles, regular sleep routines, drug therapies to improve sleep and other symptoms, and psychological tools for coping with the emotional disorders caused by the disease and for reducing stress that can exacerbate pain.
One study compared three treatment options (biofeedback and relaxation techniques; exercise; and a combination of the other two) with a passive educational approach used as a control. After two years, the combination approach proved to be most beneficial, and the passive control approach was the least.
Another study also found that interdisciplinary treatment programs were effective in significantly improving pain in 42% of patients. Improvements in pain and other symptoms, including depression and sense of physical capability, persisted for at least six months, although patients tended to become fatigued again. The effectiveness of the treatments tended to depend on how depressed the patients were, the sense of their own disability, personal support networks, and if the cause was unknown. The severity of the pain at the start of treatment had little to do with the outcome. Patients must realize that such therapies are prolonged – in some cases, lifelong – and they should not be discouraged by relapses.
Enlisting family, partners and close friends, particularly with exercise and stretching programs, and becoming involved with support groups of fellow patients are very helpful. Patients must have realistic expectations about the long-term outlook and their own individual capabilities. Improvement is subjective, and some patients are pleased with just a 10% reduction in pain and other symptoms. It is important to understand that the condition can be managed and patients can live a full life. It involves a multi-dimensional approach to treat fibromyalgia. This includes use of medications (excluding painkillers), anti-inflammatory injections, exercise sleep improvement, and maybe cognition behavioural rehabilitation programmes.
Non-Surgical Treatment For Fibromyalgia
Cognitive Therapy
Studies continue to show that when fibromyalgia patients increase their psychological capacity to deal with the specific conditions of their disorder and their lives, they are more apt to experience physical improvement. Behavioural cognitive therapy is an effective method of enhancing patients’ belief in their own abilities and to develop methods of dealing with stressful situations. A specific goal of cognitive therapy is to change the distorted perceptions that patients have of the world and of themselves; for fibromyalgia patients, this means that they learn to think differently about their pain.
Many fibromyalgia patients live their lives in extremes. They first become heroes or martyrs, doggedly pushing themselves past the point of endurance until they collapse and withdraw. This inevitable backlash reverses their self-perception, and they then view themselves as complete failures, unable to cope with the simplest task. One important aim of cognitive therapy is to help such patients discover a middle route, whereby they can prioritize their responsibilities and drop some of the less important tasks, or delegate them to others. Such behaviour will eventually lead to a more manageable life and to less of an absolutist perspective on themselves and others.
Using specific tasks and self-observation, patients gradually shift their fixed ideas that they are helpless against the pain that dominates their lives, to the perception that pain is only one negative and, to a degree, a manageable experience among many positive ones. Fulfilling experiences and many areas of control are still available. Cognitive therapy may be expensive and not covered by insurance. It should be noted that, in one centre, educational discussion groups were as effective, or even more so, than a cognitive therapy program. Such results cannot necessarily be applied to all centres; therapeutic success varies widely, depending on the skill of the therapist. The studies do indicate, however, that patients who cannot afford cognitive therapy may do as well with strong, intelligently-managed support groups.
Exercise
Many studies have indicated that exercise is the most effective component in managing fibromyalgia, and patients must expect to undergo a long-term exercise program. Some patients of fibromyalgia avoid exercise for fear it will exacerbate their pain. However, according to studies, any pain caused by exercising subsides within 30 minutes. Physical activity prevents muscle atrophy, increases a sense of well-being, and, over time, reduces fatigue and pain itself.
Aerobic Exercise
Regular low-impact aerobic exercises are the most helpful for raising the pain threshold, although it may take months to perceive benefits. A very gradual incremental program of activity, beginning with mild exercise and building over time, is important; patients who attempt strenuous exercise too early actually experience an increase in pain and are likely to become discouraged and quit. Every patient must be prepared for relapse and setbacks, which are nearly universal, but this should not dissuade the patient from exercising. Rather, they should experiment with various forms of physical activity that can be tolerated using their available energy levels. Desirable exercises are walking, swimming, and using stationary bikes. Swimming and water therapy, which eliminate weight-bearing, appear to be excellent choices for getting started. Some experts recommend the use of a training index for gauging progress and establishing a goal. This index is the product of three calculations: the duration of exercise in minutes, number of days per week that the patient exercises, and the percentage of maximum heart rate [see box]. People just beginning an exercise program should start with an index of 10 to 25 and aim over time for at least 42. As examples for achieving these goals, an initial index of 15 may be achieved with a maximum heart rate percentage of 60% during exercise performed for 5 minutes 5 times a week (.60 x 5 x 5); the later goal of an index of 42 could be achieved with a maximum heart rate percentage of 70% that occurs with 20-minute exercises three days a week (.70 x 20 x 3 = 42). (Stretching exercises should be performed for about 10 minutes before the aerobic exercise, but they are not considered part of the total exercise time that the patient uses in calculating the index goal.)
- Determining Percentage of Maximum Heart Rate
- Determine the maximum heart rate by subtracting one’s age from 220.
- Determine the heart rate by measuring the pulse either at the carotid artery on the neck or on the inside of the wrist during a workout. It is easiest to count pulse beats for 10 seconds, then multiply by 6 for the per-minute total.
- Calculate the percentage of maximum heart rate, by dividing the exercise heart rate by the maximum heart rate and multiply by 100.
Stretching Techniques
Much of the pain experienced by patients occurs where muscles join tendons or bones, particularly when the muscles are stretched. Stretching, or flexibility exercises, are part of the warm-up and cool-down routines of any regular program, but the stretching technique used for muscle relaxation and pain reduction must be performed by a person other than the patient, usually a family member or close friend. One such technique is known as “spray and stretch.” Using this method, the tender points are located by pressing on the suspected areas, which are then targeted and sprayed with either ethyl chloride (Chloroethane) or Fluori-Methane, which are chemicals that cool the blood vessels in the skin. The patient must be in a comfortable position and the face covered if the spray is being used near the head. The spray bottle is held upside-down about 12 to 18 inches from the targeted area. The spray is not used as an anaesthetic but to inactivate the tender points so that the patient’s partner can slowly stretch the affected muscle. (Anaesthetic skin creams do not appear to be effective for this treatment.) After the procedure, the muscle should feel looser, and the patient should have a greater range of motion with that muscle. In some cases, injections of lidocaine, called “trigger-point injections,” may be used for particularly painful tender points as an aid to stretching. The injection causes intense, transient pain in the trigger point, but, after the medication has taken effect, the ability to stretch the muscle is greatly enhanced. After an injection, the spray may be used on the whole muscle to inactivate less severe tender points. In some cases, injections may be needed two or three times over six to eight weeks. There is some soreness afterward, which can be severe, and the benefits of the treatment may not be apparent immediately. With use of either injections or the spray, the benefits may last from a few days to weeks. Neither the spray nor the injection is useful without muscle stretching.
Healthy Lifestyle
Establishing Regular Sleep Routines
Diet
Stress Reduction Techniques
There is some evidence that people with fibromyalgia have a more stressful response to daily conflicts and encounters than those without the disorder. A number of relaxation and stress-reduction techniques have proven to be helpful in managing chronic pain.
- Deep Breathing
Inhale slowly and deeply to the count of 10, making sure that the stomach and abdomen expand. Inhale through the nose and exhale slowly and completely, also to the count of ten. To help quieten the mind, concentrate fully on breathing and counting through each cycle. Repeat five to 10 times and make a habit of doing the exercise several times each day, even when not feeling stressed.
- Progressive Muscle Relaxation
After lying down in a comfortable position without crossing the limbs, concentrate on each part of the body, beginning with the top of the head and progressing downwards to focus on all the muscles in the body. Be sure to include the forehead, ears, eyes, mouth, neck, shoulders, arms and hands, fingers, chest, belly, thighs, calves and feet. (Some individuals even imagine tensing and releasing internal muscles once the external review is complete.) A slow, deep breathing pattern should be maintained throughout this exercise. Tense each muscle as tightly as possible for a count of five to 10 and then release it completely; experience the muscle as totally relaxed and lead-heavy. Continue until the feet are reached. In the beginning, it is useful to have a friend or partner check for tension by lifting an arm and dropping it; the arm should fall freely. Practice makes the exercise much more effective, and produces relaxation much more rapidly.
- Biofeedback
During biofeedback, electric leads are taped to a subject’s head. The person is encouraged to relax using methods, such as those described above. Brain waves are measured and an auditory signal is emitted when alpha waves are detected, a frequency that coincides with a state of deep relaxation. By repeating the process, subjects associate the sound with the relaxed state and learn to achieve relaxation by themselves.
Massage Therapy
Massage therapy is thought to stimulate the parasympathetic nervous system, which slows down the heart rate and relaxes the body. Rather than causing drowsiness, massage actually increases alertness; reduction of stress and anxiety levels and the resulting relaxation, however, do contribute to better sleep. A number of massage therapies are available for relaxing muscles, including the following:
- Shiatsu, which applies intense pressure to parts of the body, can be painful but people report deep relaxation at the end.
- Reflexology manipulates hands and feet using Eastern techniques; and
- Swedish massage has been available for years, and some experts believe is still the best method for relaxation
Extracorporeal shock wave therapy
Medical Drug Treatments
The primary goal of drug therapy is to improve sleep, but many of the medications may relieve other symptoms of fibromyalgia, including depression and low energy.
Antidepressants
Muscle Relaxing
Because fibromyalgia often develops when a woman reaches menopause, some experts believe that estrogen replacement therapy may have special benefits for fibromyalgia patients, in addition to protection against heart disease, osteoporosis and, possibly, Alzheimer’s disease. Women who take estrogen therapy seem to fall asleep faster, have longer periods of REM sleep, have fewer wakeful periods, and sleep longer than those not taking estrogen. Taking estrogen shortly before going to bed is most helpful.
Anti-inflammatory Drugs
For relief of pain, a single paracetamol may be used. Anti-inflammatory drugs, and non-steroidal anti-inflammatory drugs (NSAIDs), are less useful for the pain of fibromyalgia, since the pain is not caused by muscle inflammation. A number of patients are prescribed opioids, for pain relief. Physicians are urged to take a careful medical and psychological profile of the patient before prescribing them, and periodically evaluate the patient for continuing pain relief, side effects and indications of abuse.
Other Drugs
An interesting area of research is the use of very powerful chemicals that block pain signals to the brain. In animal studies, this combination was injected into the spinal cords of rats that were hypersensitive to pain; it relieved pain without affecting any nearby cells. Some patients have been treated with recombinant growth hormone and have experienced improvement.
Anti-convulsants
Coreflex Injections and Platelet-Rich Plasma Therapy
Coreflex injections, consisting of a mix of local anaesthetic, anti-inflammatory and muscle relaxant may be used, to reduce nerve sensitivity and relax tensed muscles of the painful areas. Platelet-rich plasma therapy has also been reported to help injured tissues heal and strengthen ligaments and reduce body pain.
Other Alternative Treatments
Because of the difficulties in treating fibromyalgia, many patients seek alternative treatments. Everyone should be wary of those who promise a cure or urge the purchase of expensive but useless and potentially dangerous treatments.
Acupuncture
Magnet Therapy
Get Your Pain Resolved
Send your enquiries or consult our pain experts today.