Trigger finger, medically known as stenosing tenosynovitis, is a condition that affects the tendons in your fingers, making it difficult to bend or straighten the affected digit. For those grappling with the discomfort and limited mobility associated with trigger finger, there are various treatment options available, one of which is trigger finger steroid injections. In this comprehensive article, we will look into the intricacies of trigger finger, its symptoms, and the effectiveness of steroid injections.
What is a Trigger Finger and What Caused It?
A trigger finger is a condition that manifests when the flexor tendon, responsible for controlling the movement of the finger, becomes inflamed. This inflammation causes the tendon to thicken, restricting its smooth gliding within the protective sheath, and results in difficulty bending or straightening the affected finger. While the symptoms are apparent, the precise cause of trigger finger is not always straightforward.
Several contributing factors can lead to the onset of trigger finger, making its etiology multifaceted. Repetitive gripping actions, commonly associated with certain occupational tasks or hobbies, create stress on the flexor tendon, potentially triggering inflammation. Moreover, individuals with pre-existing health conditions, such as rheumatoid arthritis, are more susceptible to developing trigger finger. The inflammatory nature of arthritis can also exacerbate the condition, leading to increased discomfort and reduced finger mobility.
Prolonged use of vibrating hand tools is another notable factor linked to trigger finger. Continuous vibration exposure can contribute to tendon irritation and inflammation, setting the stage for the development of this condition. Understanding these diverse triggers is pivotal in tailoring an effective treatment plan, as the underlying cause may influence the choice of interventions.
The intricate interplay of these factors highlights the importance of a thorough assessment by healthcare professionals to pinpoint the root cause of trigger finger in individual cases. By unraveling the complex web of causative elements, medical practitioners can devise targeted treatment strategies, ranging from lifestyle modifications to medical interventions like steroid injections. In essence, comprehending the nuanced relationship between inflammation, lifestyle factors, and underlying health conditions is paramount in effectively managing and alleviating the symptoms of trigger finger.
How Do I Know I Have Trigger Finger?
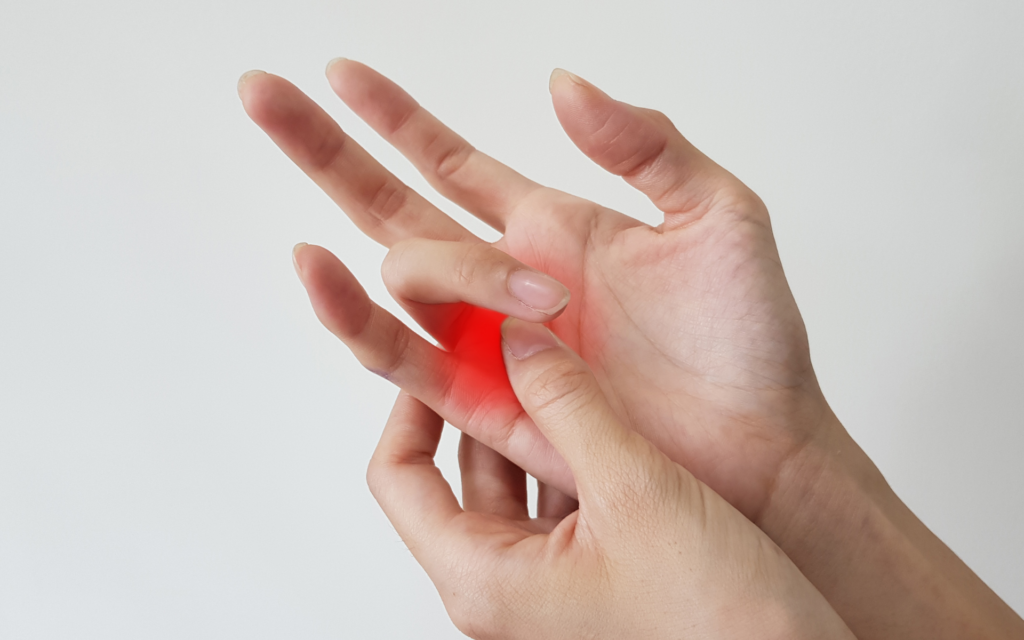
Recognition of trigger finger symptoms is paramount in initiating timely and effective treatment. The signs of this condition are diverse and can significantly impact daily activities involving hand movements. One of the primary indicators is the presence of pain or discomfort, typically localised at the base of the affected finger. This discomfort can range from mild to severe, hindering the smooth functioning of the hand.
Another characteristic symptom of trigger finger is the occurrence of a distinct clicking or popping sensation during finger movement. This audible cue is often accompanied by a tactile sensation, signaling the irregular movement of the tendon within the inflamed sheath. This phenomenon, known as “triggering,” is a hallmark of the condition and can be more pronounced in advanced stages.
Individuals with trigger finger may also experience challenges in extending or flexing the affected digit. The restricted range of motion is a direct result of the inflamed tendon struggling to glide smoothly within the tendon sheath. This limitation can interfere with routine tasks that involve gripping or grasping and may impact overall hand dexterity.
While these symptoms are indicative of trigger finger, it’s crucial to consider their persistence and impact on daily life. If the discomfort, clicking, or limited mobility persists or worsens, seeking medical evaluation becomes imperative. Doctors can conduct a thorough examination, potentially including imaging studies, to confirm the diagnosis and recommend an appropriate treatment plan.
Understanding and acknowledging these symptoms empower individuals to take proactive measures in seeking medical attention. Early intervention not only aids in managing the symptoms effectively but also prevents the progression of trigger finger to more advanced stages, where treatment options may become more complex. By staying attuned to the nuanced signs, individuals can navigate the path toward relief and restored hand functionality.
Trigger Finger vs Carpal Tunnel
Distinguishing between trigger finger and carpal tunnel syndrome is crucial in the multifaceted field of hand health because they have similar symptoms but different causes. Both disorders can impair hand function and cause pain and discomfort, but they affect different anatomical structures, so a precise diagnosis is necessary for a successful course of treatment.
Trigger finger primarily revolves around the tendons and their ability to move seamlessly within the sheath. The flexor tendon inflammation and subsequent thickening lead to difficulty in bending or straightening the affected finger. This condition is characterised by a clicking or popping sensation during movement, highlighting the involvement of the tendon-sheath interplay. Understanding this dynamic interplay is crucial for identifying trigger finger and initiating targeted interventions.
On the other hand, carpal tunnel syndrome centers around the median nerve, which runs through the carpal tunnel in the wrist. The compression of this nerve within the confined space of the carpal tunnel results in a distinct set of symptoms, including tingling, numbness, and pain radiating through the hand and fingers. Unlike trigger finger, carpal tunnel syndrome doesn’t directly impact the tendons but rather affects nerve conduction.
The ability to differentiate between these two conditions is pivotal in rendering precise diagnoses and implementing targeted treatment plans. While both trigger finger and carpal tunnel syndrome may share common symptoms, the anatomical variance underscores the need for a comprehensive examination and potentially diagnostic tests to confirm the specific ailment.
Accurate diagnosis ensures that patients receive tailored interventions, optimising the effectiveness of treatments and promoting a faster return to optimal hand function. In the realm of hand health, distinguishing between trigger finger and carpal tunnel syndrome marks a critical juncture in the journey toward informed healthcare decisions and improved quality of life.
When Should You Seek Treatment?
For the best results, it is critical to identify the symptoms of trigger finger and to seek medical attention as soon as possible. When a finger continues to hurt and you experience clicking or locking in that area, it’s time to act quickly. Postponing treatment could make the problem worse and possibly result in the formation of a permanent contracture. In advanced stages, this can limit the finger’s mobility, making non-invasive interventions less effective. Early medical assessment allows for a comprehensive evaluation of the condition’s severity and facilitates the implementation of appropriate treatments, ranging from conservative measures to more advanced interventions, thereby mitigating the risk of prolonged discomfort and functional impairment.
Why Should You Consider Coreflex Injections?
Coreflex injections comprise a combination of local anaesthetic, anti-inflammatory and muscle relaxants. It can be delivered directly into the inflamed tendon sheath, swiftly mitigating inflammation and alleviating pain associated with trigger finger. This targeted approach reduces swelling and promotes improved tendon gliding, restoring normal hand functionality.
Coreflex injections are particularly advantageous for those seeking a non-surgical alternative, providing symptomatic relief without the need for invasive procedures. The convenience and relatively quick administration of these injections make them a practical choice, allowing individuals to resume regular activities sooner. Moreover, Coreflex injections have demonstrated efficacy in various clinical studies, solidifying their standing as a reliable treatment option.
How Do Coreflex Injections Ease Trigger Finger Pain?
The mechanism through which Coreflex injections alleviate pain and stiffness is attributed to their precise delivery into the inflamed tendon sheath.
The corticosteroids in Coreflex, function as potent anti-inflammatory agents. When introduced directly into the affected tendon sheath, these steroids act swiftly to suppress the inflammatory response. This reduction in inflammation plays a pivotal role in restoring the normal gliding function of the tendon, easing the pain associated with trigger finger.
Moreover, the targeted delivery of corticosteroids minimises systemic side effects, as the medication primarily acts at the site of inflammation. This localised treatment approach enhances the safety profile of steroid injections, making them a favorable option for those seeking relief without exposing the entire body to high doses of medication.
The benefits of Coreflex Injections extend beyond mere symptom relief. By mitigating inflammation, these injections contribute to the prevention of further damage to the tendon and surrounding structures. This proactive approach not only addresses the immediate discomfort but also aids in fostering long-term hand health.
For patients considering Coreflex Injections, understanding this mechanism of action is instrumental. It empowers individuals to make informed decisions about their treatment, appreciating the targeted and effective nature of this intervention in the context of trigger finger. As a popular and proven method, steroid injections stand as a valuable tool in the arsenal against trigger finger, providing a pathway to enhanced mobility and an improved quality of life.
Are There Any Lifestyle Changes or Home Remedies that can complement trigger finger treatments?
Splinting
Adopting lifestyle changes and incorporating home remedies into the management of trigger finger can significantly enhance the effectiveness of medical interventions. One notable strategy is splinting, which involves wearing a supportive device to limit the movement of the affected finger. Splints can be particularly beneficial at night, preventing involuntary movements and promoting proper rest for the inflamed tendon. This approach aids in reducing strain and facilitating the healing process.
Finger Exercises
Targeted exercises play a crucial role in maintaining flexibility and strength in the hand and affected finger. Physical therapy exercises, can improve tendon gliding and prevent stiffness. Implementing these exercises as part of a daily routine can complement medical treatments, contributing to a more robust and sustainable recovery.
Ergonomic Adjustments
Ergonomic adjustments in daily activities are another pivotal aspect of trigger finger management. Modifying the workspace or adapting hand movements during tasks can reduce the strain on the affected tendon, minimising the risk of exacerbating symptoms. Simple changes, such as using ergonomic tools or taking regular breaks to stretch the fingers, can make a substantial difference in mitigating the impact of trigger finger on daily life.
Exploring these lifestyle changes and home remedies fosters a comprehensive and holistic approach to trigger finger management. This multifaceted strategy not only addresses the symptoms directly but also promotes overall hand health and prevents future occurrences. Individuals navigating trigger finger can collaborate with healthcare professionals to tailor these lifestyle adjustments to their specific needs, creating a personalised and effective plan for long-term well-being.
Conclusion
Navigating the realm of trigger finger treatment requires a nuanced understanding of the condition and the available interventions. From recognising symptoms to exploring the efficacy of steroid injections, this guide aims to empower individuals with the knowledge needed to make informed decisions about their healthcare.
Common FAQs
Some of the frequently asked questions on trigger finger steroid injections include:
How Long Does Coreflex Injection Last for Trigger Finger?
The duration of pain relief from Coreflex Injections can vary among individuals. On average, the effects may last anywhere from a few weeks to several months. It’s essential to consult with your doctor to determine the most suitable treatment plan for your specific case.
Are There Any Restrictions or Limitations After Coreflex Injections?
While trigger finger Coreflex Injections are generally well-tolerated, some individuals may experience temporary discomfort or swelling at the injection site. It’s advisable to avoid strenuous activities involving the affected hand immediately after the injection. Your doctor will provide personalised guidelines based on your response to the treatment.
This guide serves as a valuable resource for those exploring trigger finger treatments, shedding light on the benefits of steroid injections and empowering individuals to make informed decisions about their health and well-being.